· 4 min read
Knowledge Is Medicine: How Informed Patients Experience Better Healthcare Outcomes
In today`s healthcare system, patients are no longer passive recipients of care—they are active participants. As patients become more educated about their health conditions, treatment options, and care plans, they gain the tools necessary to make informed decisions that can significantly improve their health outcomes. Knowledge is power when it comes to better managing one`s health, reducing healthcare costs, and preventing unnecessary hospital visits.
“Each patient carries his own doctor inside him.” -Norman Cousins, Anatomy of an Illness
This powerful statement underscores the idea that patients, when empowered with knowledge, have the ability to influence their own healing process. It highlights how informed patients can be active contributors to their health and well-being, taking charge of their care and recovery.
The Power of Health Literacy
Health literacy is the ability to understand and act on health information. Unfortunately, many patients struggle to understand complex medical details, leading to poor outcomes. Low health literacy can result in medication errors, mismanaged care, and reliance on emergency services. Educating patients boosts health literacy, enabling them to manage their health more effectively, reduce complications, and lower healthcare costs.
Engaged Patients Take Control of Their Health
Education empowers patients to take an active role in their health. Patients who understand their conditions and treatment plans are more likely to adhere to prescribed care, avoid unnecessary visits, and take preventive actions. This involvement leads to better health outcomes and a more efficient healthcare system.
Chronic Disease Management: A Key Area for Education
Chronic conditions like diabetes and asthma require constant management. Patients with higher health literacy can monitor symptoms, adhere to treatment plans, and communicate better with providers, leading to fewer complications and reduced hospitalizations.
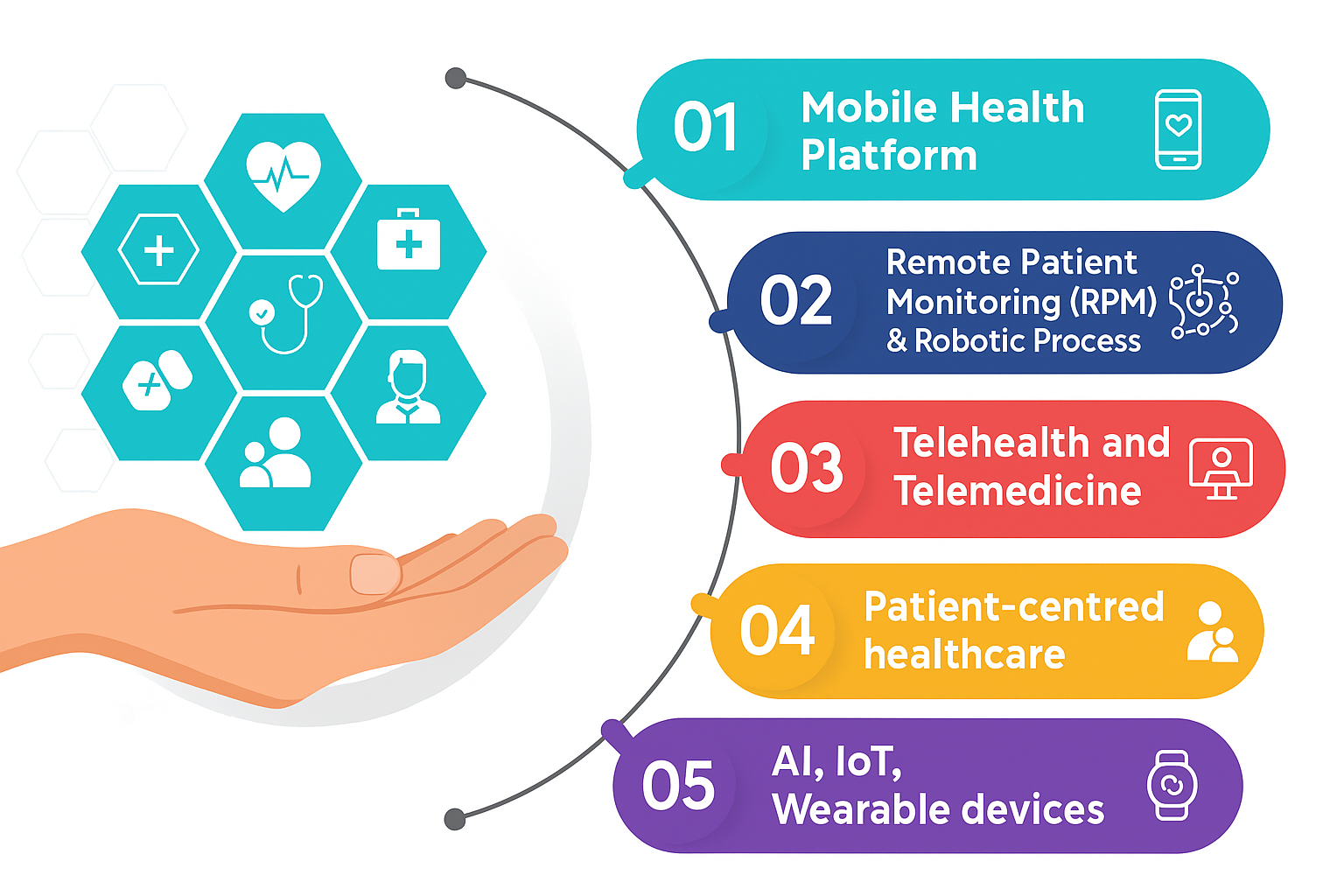
Technology as a Bridge to Better Health Education
Technology is reshaping patient education. Health apps, wearables, and patient portals provide real-time health data, allowing patients to track their health and stay informed. These tools not only support disease management but also help patients engage more actively with their healthcare providers.
Improving Healthcare Outcomes with Education
Informed patients experience better outcomes—fewer hospital visits, lower healthcare costs, and better management of chronic conditions. Increased health literacy also leads to reduced mortality rates as patients take proactive steps to manage their health.
The Role of Healthcare Providers in Education
Healthcare providers play a crucial role in patient education. By using clear, simple language and actively engaging with patients, they help ensure patients understand their health conditions and care plans. Effective communication fosters better collaboration and improved health outcomes.
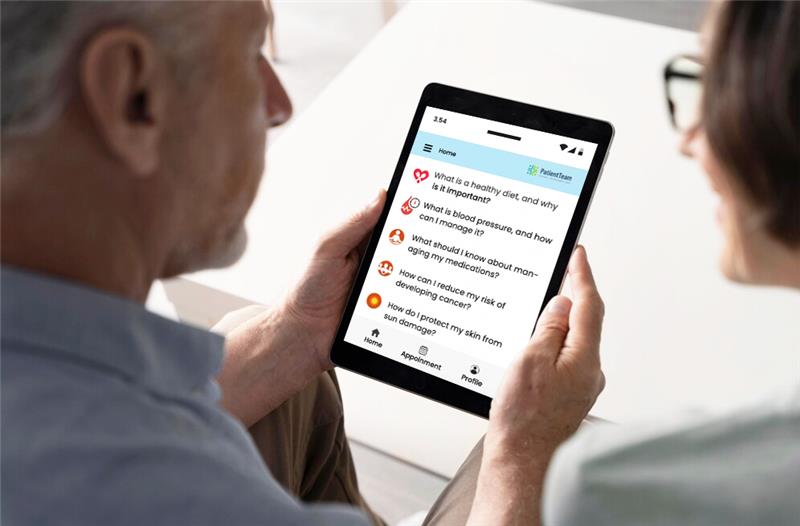
Empowering Patients with Education and Information, the PatientTeam Way

PatientTeams digital resources play a crucial role in reducing hospital readmissions. Through accessible patient portals, medication guides, condition-specific information, and educational video resources, patients are equipped with everything they need to understand their care, manage their conditions, and follow post-treatment instructions. This reduces the likelihood of complications and ensures patients are well-prepared for recovery after discharge.
The platform also provides important signposting services to guide patients to additional support and services in their community, enhancing the continuity of care beyond the hospital walls. By providing patients with these resources directly at their bedside and on their personal devices, PatientTeam not only enhances patient education but also reduces the workload on staff, freeing them to focus on more critical tasks.
Patient and Family Engagement in Healthcare
Beyond individual care, patient and family engagement is becoming a key focus in healthcare organizations and policy-making. Engagement varies across three main levels:
- Direct Care: Engagement starts with the basics—patients receive information about their diagnosis, are asked about treatment preferences, and ultimately take part in decisions that align with their preferences and the clinical judgment of their providers.
- Organizational Design and Governance: Healthcare institutions actively involve patients through surveys and advisory roles, with the highest level of engagement being when patients co-lead committees focused on improving hospital safety and quality.
- Policy Making: At the policy level, patients provide valuable input in focus groups, influence research priorities, and even share decision-making power regarding resource allocation in health programs.
The degree of patient engagement increases from consultation to shared leadership, as patients play a crucial role in shaping decisions at the personal, organizational, and policy levels. This approach enhances healthcare delivery and ensures that care aligns more closely with patients’ needs and preferences.
Conclusion
Informed patients are empowered patients. By understanding their conditions, adhering to treatment plans, and engaging in preventative care, they improve their health outcomes and reduce the burden on healthcare systems. The integration of patient education and active involvement at all levels of healthcare—from individual care to policy-making—creates a more collaborative, efficient, and patient-centered system.
Key Takeaways
- Health literacy is crucial for improving patient outcomes and reducing hospital visits and healthcare costs.
- Engaged patients take more control over their health, improving treatment adherence and overall wellness.
- Technology supports patient education by providing real-time data and improving communication between patients and providers.
- Healthcare providers must use clear communication to ensure patients understand their conditions and care plans.
- Patient engagement spans across direct care, organizational governance, and policy-making, leading to more inclusive, efficient, and patient-centered healthcare.