· 10 min read
Why Data Sharing Alone Won't Save Healthcare: The Need for Collaborative, Team-Based Care
Data sharing alone is insufficient to improve healthcare; the future lies in collaborative, team-based care that integrates diverse expertise. Digital health tools must evolve beyond data aggregation to enable real-time, seamless communication and coordination among care teams, ensuring holistic, patient-centered care that leads to better outcomes and more sustainable healthcare systems.

Data sharing has become a ubiquitous buzzword, heralded as the key to advancing improved patient outcomes and operational efficiency. The topic of data sharing has received more attention in recent years. In 1980, only 46 peer reviewed journal articles (0.0186% of the total) published in PubMed contained the keyword “data sharing”, while in 2019 there were 5960 articles (0.4253% of the total) containing this keyword. It is also interesting to see the sudden rise of interest in the subject[1] since 2016, the year of the approval of the GDPR, and another peak in 2018, the year of its enforcement.
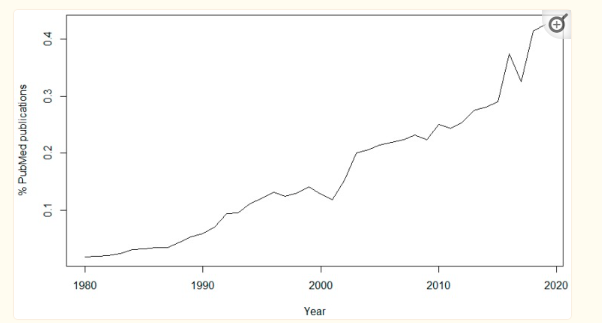
Graph of the number of abstracts of PubMed publications containing the keyword “data sharing” as a percentage of the total, per year since 1980.
However, as we look deeper into the complexities of patient care, especially in light of evolving regulatory frameworks such as Value-Based Care, New York State’s 1115 waiver, it becomes evident that data sharing, while necessary, is insufficient in isolation. The future of healthcare hinges not merely on the aggregation and dissemination of patient data but on the orchestration of collaborative, team-based care models that are adaptive, holistic, and responsive to the multifaceted needs of patients involving an entire team distributed across organizations. This integrated approach and a shift from ‘mere sharing’ and ‘aggregation’ to ‘collaboration’ seems challenging because institutions tend to believe that they own the patient data, since they collected it. However, the reality is these institutions are just “data custodians”; the data is the property of the patient and the access and use of that data outside of the clinical institute usually requires patient consent.
Adoption of Electronic Health Records (EHRs) and other digital health tools to facilitate data sharing
The healthcare industry has witnessed an exponential increase in the adoption of Electronic Health Records (EHRs) and other digital health tools designed to facilitate data sharing across various stakeholders. The logic is compelling: by ensuring that all relevant parties have access to a comprehensive patient history, we can reduce redundancies, avoid medical errors, and improve the continuity of care. However, this approach is inherently limited by its focus on data as an end rather than a means to an end. Existing communication technologies and EHR-based data sharing processes were perceived as barriers to patient care[2]. In particular, reliance on such systems and lack of interactive and holistic care-based communication among care delivery participants created obstacles to sustained thinking and discussion of care-related decision-making. Further, these systems created data overload and data fragmentation, making integration for diagnosis and care delivery difficult.
One significant challenge in relying on electronic health record (EHR) data[3] for longitudinal data collection is the difficulty in accessing data from all the locations where a patient receives care. For example, how can a study team obtain EHR data from a hospital that is not part of the participating healthcare system? If a patient experiences a heart attack while away on vacation, how will that data be captured by the study team? To address these gaps, it is often recommended to use multiple methods to gather secondary data on longitudinal outcomes, such as direct input from patients through a mobile app or call center, or by leveraging sources like administrative claims. Essentially, most important data and particularly that drives the risk assessment associated with a patient is outside EHRs.
A critical consideration when using EHR data, as opposed to collaborative working is the considerable variability in how data are recorded in EHR systems, including the different terminologies used to represent that data. This variability necessitates harmonization as an essential step in utilizing EHR data effectively. While the Office of the National Coordinator for Health Information Technology (ONC)[4] is developing a framework to enhance standardization and research capabilities within EHR systems, which would be a step toward collaboration, the adoption of these standards varies widely across the healthcare sector.
Myth: Better data sharing will automatically lead to better care
Data, in its raw form, is inert. It lacks the interpretative framework necessary to transform information into actionable insights. The assumption that better data sharing will automatically lead to better care is predicated on the belief that clinicians, once equipped with comprehensive data, will naturally arrive at the best clinical decisions. This overlooks the fact that healthcare is an inherently collaborative endeavor, requiring not just the sharing of information but the integration of diverse expertise and perspectives in real-time decision-making across institutions.
Moreover, the current emphasis on data aggregation often leads to information overload, where the sheer volume of data can obscure rather than illuminate the path to optimal care. Without a collaborative framework that contextualizes and prioritizes this data within the patient’s broader care journey, there is a risk that critical insights and action steps may be lost in the noise, leading to suboptimal outcomes of patient care.
The Case for Collaborative, Team-Based Care
The concept of team-based care is not new, yet its implementation remains inconsistent and often superficial. True collaboration in healthcare requires more than multidisciplinary teams working in parallel; it necessitates an integrated approach where communication, coordination, and shared decision-making are embedded into the care delivery process. This is particularly crucial in managing chronic conditions and addressing social determinants of health (SDoH), where the patient’s journey spans multiple touchpoints across different care settings over an extended period.
The New York State 1115 waiver[5] exemplifies the shift towards value-based care and decrease health disparities, emphasizing the need for healthcare providers to focus on overall patient outcomes. These initiatives will provide a broad swath of health and social supports to underserved communities, improving their health and quality of life. To achieve this, care must be delivered through cohesive teams that can leverage their collective expertise to address the full spectrum of a patient’s needs in supervision of social care networks[6] – who will operate as a patient’s team. These regionally based Social Care Networks (SCNs) will increase and strengthen the delivery of social care services to Medicaid members. These SCN entities will coordinate the delivery of social care services to Medicaid members by community-based organizations (CBOs), with support from shared data and technology. SCN lead entities will be charged with building reliable networks of contracted Social Service Providers to better enable HRSN (health related social needs) screening and the delivery of social care services.
In this context, digital health tools must evolve beyond their current function as repositories of data. They must become enablers of collaboration, providing the infrastructure for seamless communication and coordination among care team members to address HRSN. Each of the professionals involved in patient care as a team across institutions contributes a piece of the puzzle, but without a mechanism for integrating their inputs into a coherent care plan to deliver collaborative and real-time access, the patient is at risk of receiving fragmented and potentially conflicting care.
A team-based approach ensures that each provider’s contribution is considered in the context of the patient’s overall health status and care objectives. This not only improves the quality of care but also enhances the patient experience by reducing the burden of navigating the healthcare system independently. In this model, the patient is not merely a passive recipient of care but an active participant, with the care team providing the support and guidance necessary to achieve the best possible outcomes.
The Role of Digital Health Tools in Enabling Collaborative Care
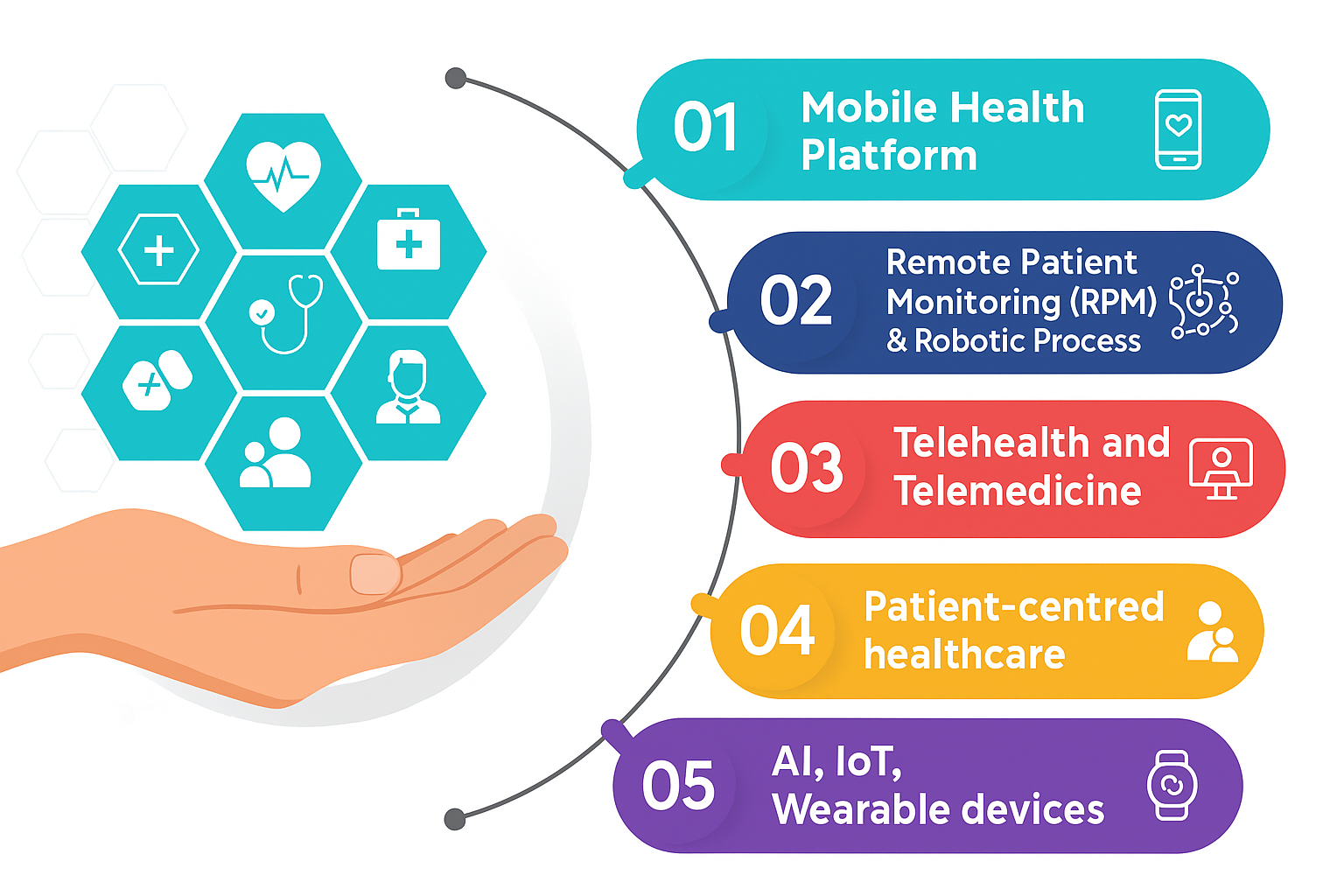
Digital health tools have the potential to be transformative enablers of collaborative care, but this potential is far from fully realized. To move beyond ‘data sharing’ and ‘data aggregation’ and embrace ‘collaborative data access’ in real-time without any need of sharing, these tools must be designed with the principles of team-based care. This involves several key considerations:
Interoperability and Integration: Digital health platforms must be interoperable across different systems and settings, allowing for seamless data exchange and integration. However, interoperability alone is insufficient. These platforms must also facilitate the integration of data into the clinical workflow, ensuring that information is not just accessible but actionable within the context of team-based care.
Communication and Coordination: Effective collaboration requires robust communication channels that support real-time interaction among care team members. Digital health tools should provide secure messaging, video conferencing, patient relationship management, and other communication functionalities that enable timely and efficient coordination of care. Moreover, these tools should support the development of shared care plans, with each team member able to contribute and update information as needed.
Decision Support and Analytics: Advanced analytics and decision support tools can help care teams make sense of the vast amounts of data generated in the healthcare process. By providing insights into patient risk factors, risk intelligence, treatment outcomes, and care gaps, next best actions, these tools can guide collaborative decision-making and ensure that care is tailored to the individual needs of each patient based on the risk intelligence.
Patient Engagement: A collaborative approach to care must also engage the patient as a central member of the care team. Digital health tools can support patient engagement by providing educational resources, self-management tools, and direct communication channels with the care team. This not only empowers patients to take an active role in their care but also ensures that their preferences and values are considered in the decision-making process.
Takeaways
The promise of digital health lies not in the ability to share more data with different entities but in the capacity to utilize and transform that data into meaningful, collaborative action. As the healthcare industry continues to evolve, particularly in response to value-based care initiatives and New York State’s 1115 waiver, the focus must shift from only data aggregation and sharing to collaboration and the delivery of coordinated, team-based care. Digital health tools that prioritize collaboration, integration, and patient engagement will be the key to realizing this vision, ultimately leading to better outcomes for patients and more sustainable healthcare systems. For healthcare leaders, the challenge is clear: to invest not just in technology but in the frameworks and processes that enable true collaboration in care delivery.
For social care networks, community-based organizations, and other collaborative care agencies looking to enhance their capabilities in delivering value-based care, Patient Team offers specialized digital health development support. Reach out to us if you are interested in creating and optimizing collaboration models for data-driven, team-based care. Let’s work together to build the frameworks that will define the future of healthcare.
Bibliography
1. Hulsen, “Sharing Is Caring—Data Sharing Initiatives in Healthcare,” NCBI, April 27, 2020
2. Quinn, Forman, Harrod, et al., “Electronic health records, communication, and data sharing: challenges and opportunities for improving the diagnostic process,” NCBI, August 27, 2019
3. Eisenstein, Anstrom, Zozus, et al., “Acquiring Electronic Health Record Data,” NIH Pragmatic Trials Collaboratory, October 14, 2022
4. “Office of the National Coordinator for Health Information Technology,” Assistant Secretary for Technology Policy, 2024
5. “CMS Approves New York’s Groundbreaking Section 1115 Demonstration Amendment to Improve Primary Care, Behavioral Health, and Health Equity,” Centers for Medicare & Medicaid Services, January 9, 2024
5. “Social Care Networks,” New York State Department of Health, August 2024