· 7 min read
From Reactive to Proactive: How Digital Health Tools Enhance Patient Engagement
In today’s rapidly evolving healthcare landscape, the traditional model of care—once dominated by reactive responses to illness—is gradually giving way to a more proactive, patient-centered approach. This shift, supported by digital health tools, encourages individuals to engage more actively in managing their health. The result is often better outcomes, improved satisfaction, and a potentially more sustainable healthcare system.
Reactive vs. Proactive Care: Defining the Difference
Reactive care primarily focuses on treating illness and addressing symptoms after they arise. Patients typically interact with healthcare providers when health problems become acute—such as visiting a doctor for a new symptom or an emergency room in the case of sudden illness.
By contrast, proactive care aims to prevent disease, detect conditions early, and maintain ongoing management through continuous engagement. This approach leverages regular monitoring and personalized interventions designed to keep patients healthier and reduce the need for urgent care. Digital technologies like wearable devices, health apps, and AI-driven platforms have made it increasingly feasible to track health data in real time and encourage timely, informed actions.
Challenges of Patient Disengagement in Traditional Models
Despite its importance, patient engagement has long been a challenge in conventional healthcare settings. Limited interaction time with providers, difficulty accessing relevant health information, and the complexity of care pathways can leave patients feeling disconnected or overwhelmed. This disengagement may contribute to poor adherence to treatment plans, delayed care seeking, and ultimately preventable health complications.
Furthermore, reactive models tend to allocate significant resources to managing chronic diseases and mental health conditions after they have progressed. In countries like the U.S., this focus contributes to substantial healthcare expenditures, with preventable hospitalizations alone costing billions annually and putting considerable strain on health systems. These patterns highlight the potential benefits of shifting toward models that prioritize early intervention and prevention.
Empowering Engagement Through Digital Health Tools
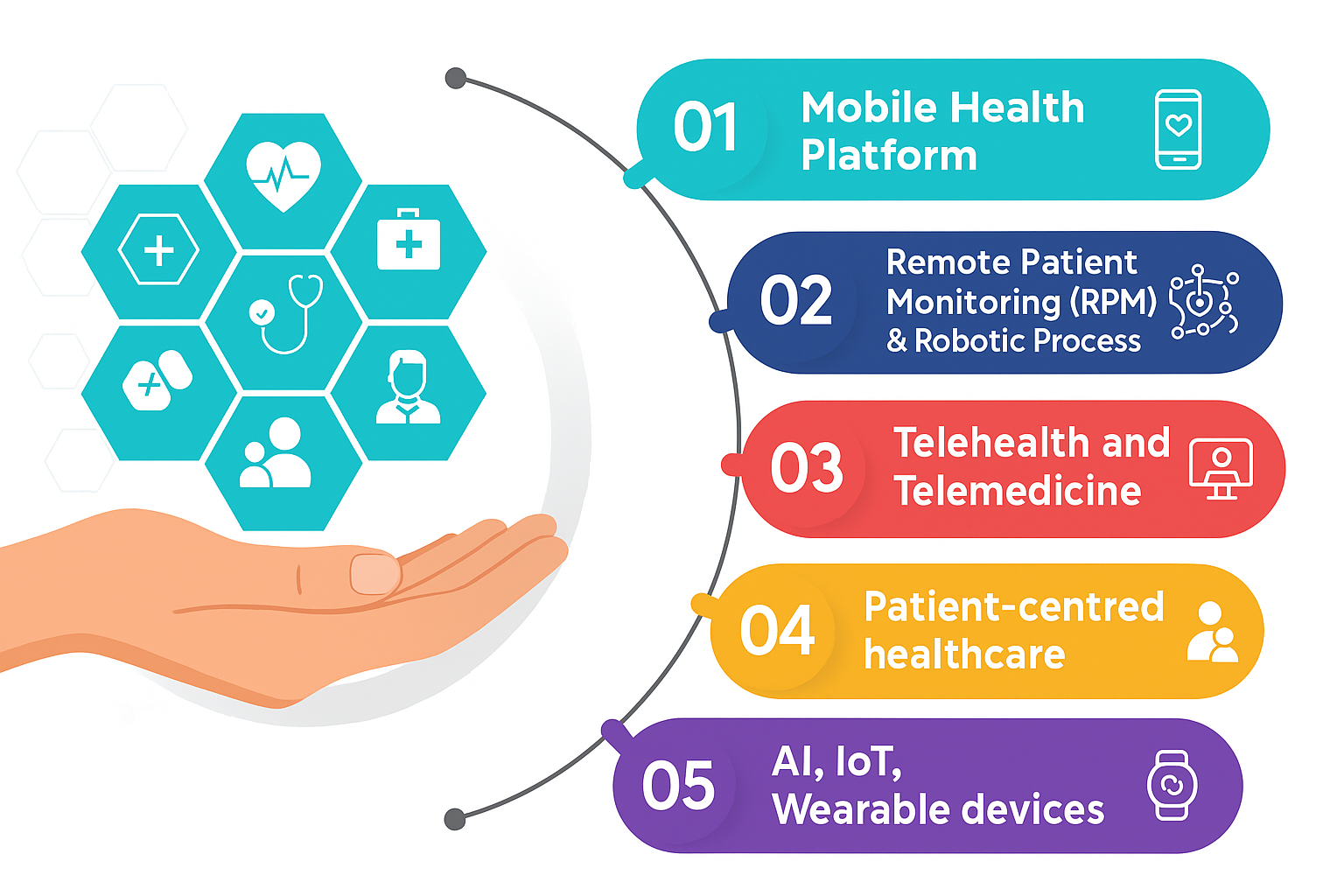
Digital health technologies are increasingly positioned as tools to bridge gaps between patients and providers by facilitating ongoing, accessible communication and personalized support. These include:
- Remote Monitoring Devices: Wearables and connected tools continuously collect health metrics—such as heart rate or blood glucose levels—offering timely insights that can prompt early interventions.
- Patient Portals: Secure online platforms grant patients access to their medical records, test results, and the ability to communicate with care teams conveniently.
- Mobile Health Apps: From medication reminders to symptom tracking and wellness guidance, these apps encourage daily self-care and build long-term health habits.
- AI-Powered Chatbots and AI Powered Virtual Assistant: Available around the clock, chatbots provide health information, basic triage, and behavioral support, expanding access beyond traditional office hours.
- Telehealth Services: Virtual consultations remove geographic and logistical barriers, enabling more frequent follow-ups and chronic disease management.
These technologies not only improve access and convenience but also contribute to education and empowerment. By equipping patients with relevant, real-time information, digital tools encourage more informed decision-making and foster a stronger sense of partnership with healthcare providers.
Smart Hospitals and Age-Tech: Innovating for Better Patient Experiences
Hospitals are embracing digital transformation by integrating technologies across clinical and administrative workflows. Smart hospitals connect digital and physical assets throughout care delivery—from registration to clinical treatment—creating a unified system that improves data sharing, accelerates workflows, and enhances patient experiences. This connectivity supports more proactive, precise care and faster adoption of new innovations.
Alongside this, Age-Tech—technology designed with older adults in mind—is becoming increasingly important. It includes tools that help seniors manage health and stay connected, such as medication reminders and family care coordination apps. As more digitally familiar baby boomers age, demand for Age-Tech that fits their lifestyles grows, highlighting the need for accessible infrastructure like reliable home internet.
Together, smart hospitals and Age-Tech demonstrate how healthcare is evolving toward more connected, personalized, and proactive models that better serve patients across all stages of life.
Incentivizing Preventive and Proactive Care
The integration of proactive digital engagement aligns with evolving healthcare policy trends that reward quality and prevention. For instance, systems like the U.S. Medicare Advantage star ratings assess health plans based on preventive care delivery, chronic disease management, and patient satisfaction. Plans that score well on these measures often receive increased reimbursements and enjoy better patient retention.
Such frameworks highlight how financial incentives can encourage healthcare providers and payers to move beyond reactive treatment, supporting models that emphasize early intervention and holistic wellness. While these policies are most developed in some countries, their principles offer valuable lessons for healthcare systems worldwide seeking to promote sustainability and patient-centered care.
Tangible Benefits and Real-World Impact
The shift toward proactive care, enabled by digital engagement, has shown promising results. For example, in a large healthcare system’s remote monitoring program for heart failure patients, connected devices tracked weight and blood pressure daily. This data allowed clinicians to detect early signs of deterioration and intervene before hospitalization was needed. The program led to a significant reduction in hospital readmissions and increased patients’ confidence in managing their conditions.
Beyond clinical outcomes, digital tools also improve the overall patient experience by making care more personalized, timely, and convenient. Patients often report higher satisfaction when they feel actively involved and supported in their health journeys.
The Future: A More Personalized, Participatory Healthcare Model

Looking ahead, digital health is poised to further transform care delivery and patient engagement. Advances in predictive analytics, genomics, and artificial intelligence will allow even greater customization of preventive strategies and interventions tailored to individual risk profiles.
Our health prospects are influenced by many factors including genetics, environment, diet, stress and exercise levels, lifestyle, and socioeconomic status. These variables mean that two patients with the same illness may respond differently to identical treatments. Recent medical advances, such as genomics and immunotherapy, have enabled healthcare professionals to better understand an individual’s predisposition to certain illnesses and to develop more targeted therapies. This more personalized approach, often referred to as precision medicine, has already contributed to improved patient outcomes.
However, customized treatments are only one facet of personalized healthcare. A broader vision is emerging that places personalization at the core of a patient-centric model—one focused not only on treatment but also on prevention and risk prediction at both individual and population levels. This evolving framework, sometimes called the 6P model, encompasses care that is Personalized, Participatory, Preventive, Predictive, Precision-driven, and Population-oriented.
By recognizing individual variability and leveraging technological advancements, this model supports a shift toward proactive, participatory care where patients are more engaged and empowered to take control of their health. As healthcare systems continue to evolve, these principles will likely shape the future of medicine, emphasizing both better outcomes and more meaningful patient involvement.
Conclusion
The progression from reactive to proactive care is more than a technological shift; it represents a fundamental cultural change in how health and wellness are understood and managed. Digital health tools, by enhancing access, education, and continuous engagement, are facilitating this transformation. Similarly, advancements in AI, the Internet of Things (IoT), and machine-to-machine communications are enabling healthcare organizations to streamline clinical development and supply chain processes, making them faster and more efficient.
This surge in data accumulation and processing power represents a transformational opportunity for patient care to become more precise, predictive, personalized, and convenient. While the future will undoubtedly bring new challenges and opportunities, fostering patient-centered digital engagement holds promise for improving health outcomes and building more sustainable healthcare systems worldwide.
Key Takeaways
- The shift from reactive to proactive care emphasizes prevention, early intervention, and continuous patient engagement, moving beyond traditional models focused mainly on treating illness after symptoms appear.
- Digital health tools—including remote monitoring devices, patient portals, mobile apps, telehealth, and AI-powered platforms—play a pivotal role in empowering patients to actively manage their health and fostering stronger patient-provider collaboration.
- Personalization, informed by advances in genomics, predictive analytics, and precision medicine, is central to the future of healthcare, enabling tailored prevention and treatment strategies that reflect individual variability.
- Emerging technologies such as AI, IoT, and machine-to-machine communications not only enhance clinical and operational efficiency but also facilitate more precise, predictive, and convenient care delivery.
- Adopting patient-centered digital engagement models has the potential to improve health outcomes, increase patient satisfaction, and support the sustainability of healthcare systems worldwide.